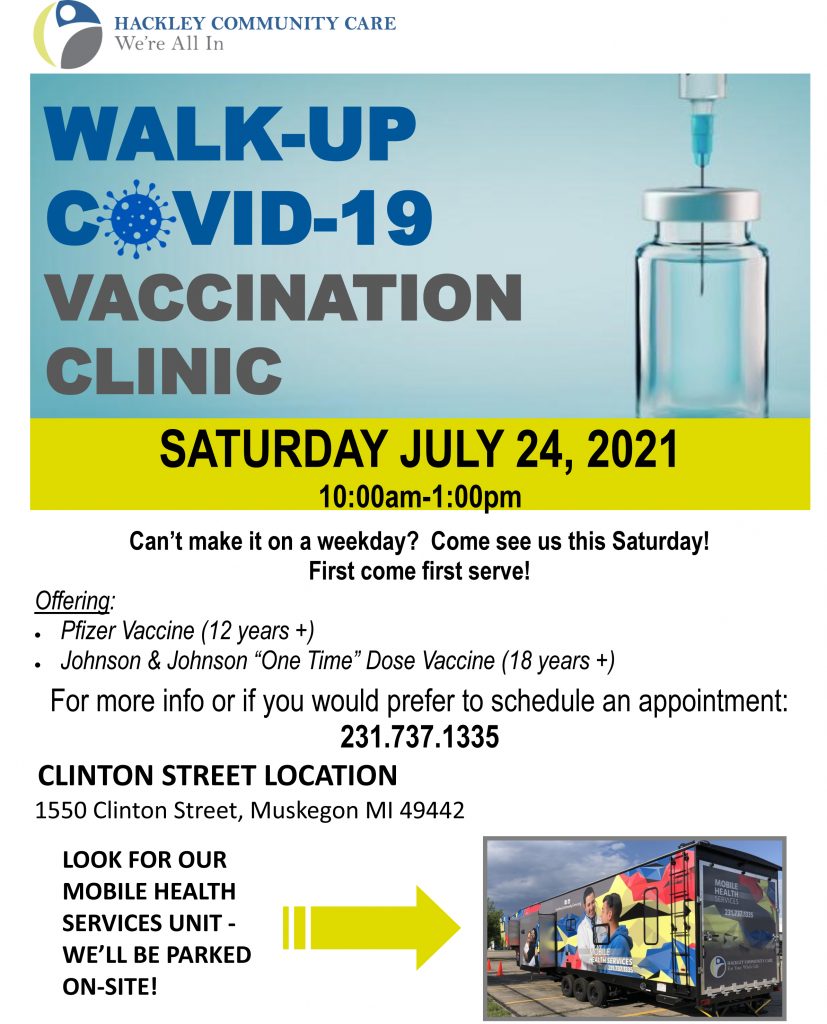
Walk-Up COVID-19 Vaccine Clinic – Saturday, July 24

submitted by the Ottawa County Department of Public Health
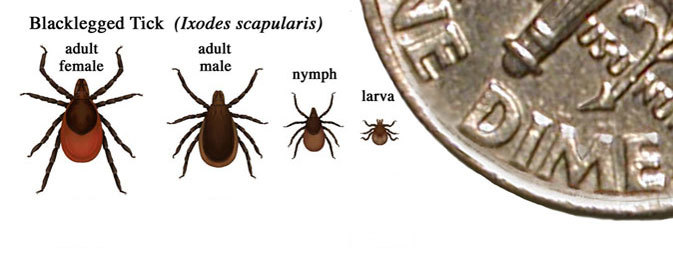
In Michigan, there’s a significant increase in the number of ticks this year. Several reports of Lyme disease have been detected. Lyme disease is the most commonly reported tick-borne disease. It is spread by an infected blacklegged (deer) tick. Most humans are infected through the bites of immature ticks called nymphs that feed during the spring and summer months. Nymphs can be difficult to see since they are approximately the size of a poppy seed. In most cases, the tick must be attached for 36 to 48 hours or more before the Lyme disease bacterium can be transmitted. “Prompt removal of ticks is the best method to decrease the chance of Lyme disease,” said Dr. Paul Heidel, the medical director of the Ottawa County Department of Public Health. “Seek medical attention if you develop a fever, a rash, severe fatigue, facial paralysis, or joint pain within 30 days of being bitten by a tick.”
The most important way to protect against Lyme disease is to prevent tick bites.
Avoid direct contact with ticks
Use insect repellent
Find and remove ticks

“Tick checks are recommended after any outdoor activities in grassy, brushy, or wooded areas. Check your clothing, body and pets for ticks when you return home,” said Adeline Hambley, the Environmental Health Manager at Ottawa County Department of Public Health.
For more tick and Lyme disease information, please visit www.cdc.gov/lyme or see the CDC Hikers/Campers Lyme Disease Fact Sheet. Please also visit www.michigan.gov/lyme or view the MDHHS Guide to Preventing Tick-Borne Illness.
Behavioral Health Services Discontinued at Muskegon Covenant Academy
MUSKEGON Mich. — Hackley Community Care (HCC) School Based Health Programs behavioral health services at Muskegon Covenant Academy, ended on May 7, 2021.
HCC’s School Based Programs provided behavioral health counseling to students at Covenant Academy who are pursuing high school completion in a more flexible, non-traditional education environment, for the past 5 years.
HCC’s School Based Health Programs is committed to continuing services to Covenant Academy students and their families at one of our other locations listed below.
Students also have the option to receive services at one of our other convenient locations within Muskegon County.
Our staff at the Muskegon Teen Health Center are available to help coordinate continued and or new services for students and their family. Appointments can be scheduled by calling the Muskegon Teen Health Center at 231.733.6680.
It has been a privilege working with the students, families and staff at Muskegon Covenant Academy. We look forward to providing continued service to you at one of the above listed HCC locations.
submitted by Jamie Hekker, Community Engagement Coordinator, Public Health – Muskegon County
Muskegon, MI – Public Health – Muskegon County continues to investigate all positive cases of novel coronavirus (COVID-19) in Muskegon County. As anticipated, cases have been identified in employees and residents of residential congregate facilities such as long term care, assisted living, and adult foster care. No further information about the residents or employees will be released due to privacy laws.
“Because residents of these types of facilities are typically elderly and many have medical conditions,” explained Kathy Moore, Muskegon County Health Officer, “they are at higher risk of becoming sick with many illnesses including COVID-19.”
Public Health – Muskegon County works closely with long term care, assisted living, and adult foster care facilities to ensure they are aware of infection control practices and knowledgeable of Muskegon Department of Health and Human Services (MDHHS) and Centers for Disease Control (CDC) guidance. Their diligent efforts to protect those most vulnerable and their cooperation with PHMC on the ongoing response to this pandemic are greatly appreciated.
Residential congregate facilities are proactively working to protect their vulnerable residents and their staff by:
• Monitoring employees and residents for symptoms of respiratory illness.
• Limiting activities within their facilities.
• Requiring residents to quarantined in their rooms.
• Restricting all visitors to the facility.
• Enhancing use of personal protective equipment for staff.
• Increasing cleaning and disinfection routines.
“COVID-19 is present in our community,” reminded Moore. “To help protect those most vulnerable, especially those in assisted living and long term care, we need everyone to do their part to minimize the spread of this virus in our community.”
Everyone should continue to follow recommendations:
• Stay at home as much as possible. Only go out for essentials like groceries or for medical emergencies.
• If you must go out, stay six feet away from others and wear a cloth face covering
• Wash your hands often and try not to touch your face or mouth
• Cover your coughs and sneezes and call your doctor for guidance if you become sick.
issued by Citizens Commission on Human Rights of Florida

In 1976, California was the first State to recognize the dangers of electroshock—and prohibited its use on children under the age of 12. More than 40 years later, the FDA has failed to ensure clinical trials prove that ECT devices are safe and effective.
CCHR’s latest documentary is a wake-up call to protect 100,000 people, including children, pregnant women and the elderly from electroshock treatment.
CLEARWATER, FLORIDA, UNITED STATES, November 25, 2019 /EINPresswire.com/ — The Citizens Commission on Human Rights (CCHR) International’s latest documentary, “Therapy or Torture: The Truth about Electroshock” aired on the Scientology TV Network over the weekend and is now part of a series of compelling award-winning CCHR documentaries available on the station. Electroshock, also known as electroconvulsive therapy (ECT), is the passage of up to 460 volts of electricity sent through the brain causing a grand mal seizure. Psychiatrists admit they don’t how it “works” and that it cannot cure, but 100,000 Americans and over 1 million worldwide are administered it every year. The documentary flanks CCHR’s campaign to have ECT banned as outmoded and dangerous. An online petition has nearly 110,000 supporters.
Craig Newnes, a clinical psychologist and author of A Critical A-Z of Electroshock!, is one of many experts interviewed for the documentary. He calls the treatment “electrocution. That’s all it is. They don’t call it electrocution; they call it Electroconvulsive Therapy because it has a magic three letter acronym, E-C-T. And one thing it isn’t is a therapy.”
He further states: “The outcome of that is it destroys brain cells. And the more brain cells you destroy, in theory, the better it is for the person. The biggest mystery of all is why on earth people think that putting bolts of electricity through people’s heads is a good idea.”
Jonathon Emord, a constitutional attorney who is challenging the U.S. Food and Drug Administration (FDA) over its classification of the ECT devices, says ECT “is ultimately imparting large amounts of electricity, many times the voltage you would get even if you stuck your finger into a light socket.” The mental health industry doesn’t “deny that there are disadvantages to ECT,” but “they minimize them. It’s a sales pitch.”
“This is an atrocity, and the FDA does nothing. They need to be held accountable while governments override them and ban electroshock in mental health practice.”
— Jan Eastgate, international president of CCHR
Some of that pitch is that anesthetics and muscle relaxants now given before ECT is administered, lessens the risk of breaking bones and trauma. But Fred Shaw, an international spokesperson for CCHR and former law enforcement officer said, “If you are awake and get hit with a baseball bat, it’s obvious that you would feel a lot of pain. But if you’re unconscious and get hit with a baseball bat, your body goes through that same trauma. So why are psychiatrists arguing that the body doesn’t go through trauma just because somebody’s unconscious? It’s assault and battery.”
Dr. Genevieve King, a physician, explains in “Therapy or Torture”: “The more seizures a person has, the more potential there is for cognitive decline, different neurologic dysfunctions and more and more seizures.” Adds neurologist Dr. Ken Sharlin: “Having recurrent seizures potentially reduces the life span of that individual. It has an impact on mortality.” He observed ECT being administered during his medical training, thinking even then, it was “barbarian.” He says: “I thought it was truly one of the most obnoxious things I’d ever seen done to a human being. A huge percentage of these people have brain damage.”
The documentary includes archival and current footage of ECT being given with patient testimony from electroshock survivors, including:
• “I went through a neurocognitive testing six months after and I lost approximately about 50 points of IQ”;
• “I didn’t remember my name, I didn’t remember anything. I didn’t remember what happened the day before. I didn’t remember anything at all”; and
• “I was pretty much tortured. I was being forced to have this treatment. I didn’t like it, I didn’t want it. And when I was honest with the doctors about how it affected me and I told them, they just interpreted that as part of my depression…. What was done to me was really, frankly, evil.”
Manfred Nowak, a former U.N Special Rapporteur is interviewed, stating: “Against-your-will electroshock therapy is in my opinion absolutely prohibited” and constitutes “torture.” A July 2018 U.N. Human Rights Council report called on governments to recognize that forced psychiatric treatment, including ECT, are “practices constituting torture or other cruel, inhuman or degrading treatment or punishment….”[1]
In 1976, California was the first State to recognize the dangers of electroshock—and prohibited its use on children under the age of 12. More than 40 years later, the FDA has failed to ensure clinical trials prove that ECT devices are safe and effective. Yet, in October, 2018, the manufacturer of one ECT device warned of “permanent brain damage” is a potential risk.[2] This followed a California lawsuit which had recently settled. The attorney representing the plaintiffs in that case wrote: “the United States District Court for the Central District of California ruled that there was sufficient evidence for a reasonable jury to find that the prominent manufacturer of ECT devices…caused brain injury in the plaintiffs by failing to warn their treating physicians of the risk of brain injury associated with ECT.”[3]
Jan Eastgate, international president of CCHR, who has documented hundreds of cases of ECT damage, says: “This is an atrocity, and the FDA does nothing. They need to be held accountable while governments override them and ban electroshock in mental health practice.” She urges ECT survivors and their families to report electroshock abuse to CCHR.
CCHR, the mental health industry watchdog, was established by the Church of Scientology and renowned professor of psychiatry and author, Dr. Thomas Szasz in 1969 to investigate and expose abuses in the mental health system. L. Ron Hubbard, founder of Scientology, first brought psychiatric imprisonment to wide public notice: “Thousands and thousands are seized without process of law, every week, over the ‘free world’ tortured, castrated, killed. All in the name of ‘mental health,’” he wrote in March 1969. For more information visit www.cchrflorida.org.
References:
[1] “Mental health and human rights: Promotion and protection of all human rights, civil, political, economic, social and cultural rights, including the right to development,” Annual report of the United Nations High Commissioner for Human Rights and reports of the Office of the High Commissioner and the Secretary-General, Human Rights Council, 10-28 Sept. 2018, p. 14, point 46
[2] www.madinamerica.com/2018/11/ect-manufacturer-warns-permanent-brain-damage/; www.thymatron.com/catalog_cautions.asp
[3] David Karen, “ECT Litigation Update: Are Patients Being Warned of Brain Damage Risk?” MAD, 13 June 2019, www.madinamerica.com/2019/06/ect-litigation-patients-not-warned-brain-damage-risk/.
Diane Stein
Citizens Commission on Human Rights of Florida
+1 727-422-8820
email us here
Visit us on social media:
Facebook
Twitter
LinkedIn
Hackley Community Care a nationally ranking community health center announces new Chief Medical Officer appointment.
 Muskegon, MI – Hackley Community Care is pleased to announce that Dr. Leslie Kingsley, MD, has been appointed the new Chief Medical Officer for Hackley Community Care. Dr. Kingsley joined Hackley Community Care in 2015 as a family practice physician.
Muskegon, MI – Hackley Community Care is pleased to announce that Dr. Leslie Kingsley, MD, has been appointed the new Chief Medical Officer for Hackley Community Care. Dr. Kingsley joined Hackley Community Care in 2015 as a family practice physician.
Dr. Leslie Kingsley, DO, received her medical degree from Michigan State University College of Osteopathic Medicine and her Bachelors of Biomedical Science Degree from Grand Valley State University. She completed her family practice residency at Munson Medical Center in Traverse City, MI.
Dr. Kingsley is a National Health Service Corps Scholar and has served as a volunteer for the American Red Cross, Grand Traverse Health Clinic, and worked as an education coordinator with AmeriCorps Together We Prepare in Grand Rapids, MI. She practices full spectrum family medicine by seeing patients of all ages, and she has a particular interest in using osteopathic medicine and principles in her patients’ care.
She likes to travel and explore, but has always had a love for Western Michigan.
About Hackley Community Care
Hackley Community Care (HCC) is a Federally Qualified Health Center that has been providing quality health care services since 1992. Hackley Community Care has continuously expanded to provide an array of services that include full primary care, dental, behavioral health, pharmacy (Community Care Pharmacy), home based and school based health services, and other supporting programs such as Grandparents Raising Grandchildren, Komen Breast Health, and BCCCNP services, to name a few. All of our services are designed to meet the needs of the underserved in our community.
Hackley Community Care was recently recognized as ranking among the top 30% of health centers nationally for clinical quality by the Health Resources and Services Administration (HRSA), Advancing Health Information Technology (HIT) for Quality from HRSA and MQIN Champion Highest Achiever award by Michigan Primary Care Association (MPCA)
Learn more about HCC at hackleycommunitycare.org
Summary report predicts homelessness, poverty, increased incarceration and deaths
March 29,2019 – The Community Mental Health Association of Michigan (CMHAM) today released a new analysis, “Systemic Underfunding of Michigan’s Public Mental Health System,” which studies the longstanding underfunding of Michigan’s public mental healthcare system. The study cites a $150 million gap between the cost of health care and the funding provided to Michigan’s public mental health system. The need and cost for services provided by HealthWest (the Community Mental Health for Muskegon County) has been increasing each year. HealthWest is serving an average of 15% more people each year, over the past five years. The intellectually and developmentally disabled population served by HealthWest grows by an average of 7% each year. This population requires the highest-cost services. Despite extensive growth in the demand for services, revenue over the past five years has only grown by an average of 1.67% per year. In addition to the growing population served by HealthWest, expenses per person served have also increased by an average of 2.75% annually.
CMHAM’s analysis makes five concrete recommendations to address the current crises in unmet mental health and substance use disorder needs – recommendations that, if followed, will stem homelessness, poverty, incarceration and the premature death of Michiganders with intellectual and developmental disabilities, mental illness, and substance use disorders.
“Michiganders do not face the same mental health and substance use disorder needs that they had 20 years ago,” said Robert Sheehan, the CEO of the CMHAM (formerly the Michigan Association of Mental Health Boards). “There are new demands, new crises and new conditions in every community throughout Michigan, which the original financing structure did not account for. These include the opioid crisis, incarceration of those with mental health needs, the recognition of the prevalence of autism, increased homelessness and more—yet the system is still operating from a decades old funding structure. This is the reality that the public mental health system in Michigan has faced for decades. Without moving toward the ambitious vision outlined by the Association and addressing this outdated funding structure, Michiganders will continue to live without the mental health care that they need and expect.”
“HealthWest is doing more with less. We have reduced expenditures by increasing caseload size and cutting administrative costs.” said Julia Rupp, HealthWest Executive Director. “Our staff are working hard to provide the best quality care to everyone who comes through our doors.” HealthWest spent an average of $14,372 per consumer in FY2015. That decreased 26% to $10,576 in FY2018. HealthWest has seen significant increases in service requests for Muskegon County youth as well as individuals with substance use disorders. Muskegon County is home to 13% of the region’s population, but accounted for 38% of the region’s Substance Use Disorder admissions last year.
For more information on the reports mentioned, visit https://cmham.org/systemic-underfunding-of-michigans-public-mental-health-system/ . To get involved in your local community visit www.healthwest.net
Currently 8 million U.S. children are being prescribed psychiatric drugs, with more than 1 million between the ages of zero to five.
from EINPresswire.com
CLEARWATER, FLORIDA, UNITED STATES, December 18, 2017 — The Citizens Commission on Human Rights (CCHR) of Florida, a non-profit mental health watchdog dedicated to protection of children, is calling for an investigation into the heavy psychiatric drugging of children; especially foster children, in Florida.
“Children are being drugged simply because psychiatry has reclassified normal childhood behaviors and repackaged them as ‘mental disorders’ resulting in the psychiatric drugging of millions of kids.”
— CCHR
A report from the research arm of Florida’s child-protection system released in 2015 showed that foster children are being put on psychotropic medications without caregivers following proper procedures and that 11 percent of the children in foster care had active prescriptions for at least one psychotropic drug. While a review of 140 children’s files showed just 20 percent of these children met all the key requirements for administering such medication.
Following the tragic death of 7-year-old Gabriel Myers in 2009, who was found hanging from a shower fixture in his foster home after having been prescribed two “black box” drugs intended for adults – the Florida policies for using psychotropic drugs on foster kids were updated but this has not solved the problem.
The psychiatric drugging of children is not just confined to the foster care system. In 2011 a two-year investigation concluded that kids in Florida, Massachusetts, Michigan, Oregon and Texas were “prescribed psychotropic drugs at rates 2.7 to 4.5 times higher than other children in Medicaid in 2008.”
Currently 8 million U.S. children are being prescribed psychiatric drugs, with more than 1 million between the ages of zero to five. Children are being drugged simply because psychiatry has pathologized normal childhood behaviors, and repackaged them as “mental disorders.” The result is that millions of children are being drugged for behaviors reclassified by psychiatry as “disease.”
As a result, CCHR is calling for an investigation into the psychiatric drugging of children in the United States. Individuals are invited to the center, located at 109 N. Fort Harrison Avenue in downtown Clearwater, to learn more about the dangers associated with psychiatric drugs as well as alternatives to medication. To learn more, please call 727-442-8820 or visit www.cchrflorida.org.
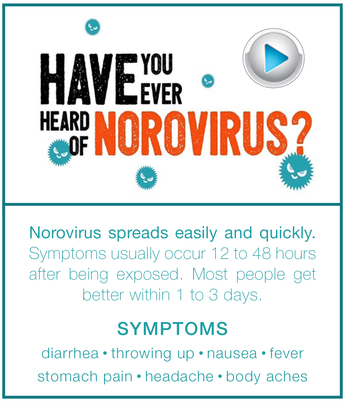 Having direct physical contact with a person who is infected, such as caring for or shaking hands with a sick person and then touching your hands to your mouth.
Having direct physical contact with a person who is infected, such as caring for or shaking hands with a sick person and then touching your hands to your mouth.
Eating food or drinking liquids that are contaminated with norovirus.
Touching surfaces or objects with norovirus on them and then putting your hands in your mouth.
People with norovirus illness are most contagious from the moment they begin feeling ill and for the first few days after they recover. Some people may be contagious for even longer.
“We are receiving an increase in stomach virus reporting. Primary outbreaks are within school and childcare settings. To reduce the risk of illness in our community, people need to take preventive measures to stay healthy,” said Marcia Mansaray, epidemiologist.
Protect Yourself and Others from Norovirus
• Wash hands with soap and water, especially after using the toilet and changing diapers – and always before eating or preparing food. Hand sanitizers are generally not effective for norovirus
• Handle and prepare food safely. People with norovirus illness should not prepare food for others while they have symptoms and for at least two days after they recover from their illness.
• Clean and disinfect contaminated surfaces (such as toilets, counters and doorknobs). Always clean up the entire area immediately after someone with norovirus vomits or has diarrhea. Put on disposable gloves and disinfect contaminated surfaces using a bleach-based household cleaner as directed on the product label or with a solution of five tablespoons of bleach to a gallon of water.
• Wash laundry thoroughly. Immediately remove and wash clothing or linens that may be contaminated with vomit or stool. Handle soiled items carefully – try not to shake them – to avoid spreading the virus. If available, wear disposable gloves while handling soiled clothing or linens and wash your hands after handling.
• Stay home if sick for at least 24 hours after symptoms end to avoid spreading the illness to others.
For more information, visit www.cdc.gov/norovirus.
Ann Arbor, MI – October 13, 2017 – November is National Alzheimer’s Disease Awareness Month and National Family Caregivers Month. The Alzheimer’s Association is marking these events by recognizing and honoring the more than 15 million family members and friends across the U.S. who are currently caring for a person living with Alzheimer’s.
According to a recent Alzheimer’s Association survey, people overwhelmingly agree (91 percent) that caring for someone with Alzheimer’s or another form of dementia should be a group effort among family or close friends, yet one out of three caregivers are not engaging others in caregiving tasks. More than four in five caregivers would have liked more support in providing care for someone with Alzheimer’s or another form of dementia, especially from their family. With 15 million Alzheimer’s caregivers across the country, that leaves a lot of people in need of support.
This November during National Family Caregivers Month, the Alzheimer’s Association is encouraging people to lend a hand to caregivers. Here are some ways that you can help.
Learn: Educate yourself about Alzheimer’s disease – its symptoms, its progression and the common challenges facing caregivers. The more you know, the easier it will be to find ways to help. The Alzheimer’s Association has a vast amount of resources and information available at www.alz.org.
Build a Team: The Alzheimer’s Association Care Team Calendar is a free, personalized online tool to organize family and friends who want to help with caregiving. This service makes it easy to share activities and information within the person’s care team. Helpers can sign up for specific tasks, such as preparing meals, providing rides or running errands. Users can post items for which assistance is needed. Visit the Care Team Calendar here: www.alz.org/care/alzheimers-dementia-care-calendar.asp.
Give a Break: Make a standing appointment to give the caregiver a break. Spend time with the person with dementia and allow the caregiver a chance to run errands, go to their own doctor’s appointment, participate in a support group or engage in an activity that helps them recharge. Even one hour could make a big difference in providing the caregiver some relief.
Check In: Almost two out of every three caregivers said that feeling isolated or alone was a significant challenge in providing care for someone with Alzheimer’s or another form of dementia. What’s more, half of all caregivers felt like they couldn’t talk to anyone in social settings or work about what they were going through. So start the conversation – a phone call to check in, sending a note, or stopping by for a visit can make a big difference in a caregiver’s day and help them feel supported.
Tackle the To-Do List: Ask for a list of errands that need to be run – pick up groceries, dry cleaning or even offer to shuttle kids to and from activities. It can be hard for a caregiver to find time to complete these simple tasks outside of the home that we often take for granted.
Be Specific and Be Flexible: Open-ended offers of support (“call me if you need anything” or “let me know if I can help”) may be well-intended, but are often dismissed. Try making your offer of help or support more specific (“I’m going to the store, what do you need?” or “I have free time this weekend, let me stop over for a couple of hours so you can do what you need to do.”) Don’t get frustrated if your offer of support is not immediately accepted. The family may need time to assess its needs. Continue to let the caregiver know that you are there and ready to help.
Help for the Holidays: Holiday celebrations are often joyous occasions, but they can be challenging and stressful for families living with Alzheimer’s. Help caregivers around the holidays by offering to help with cooking, cleaning or gift shopping. If a caregiver has traditionally hosted family celebrations, offer your home instead.
 Join the Fight: Honor a person living with the disease and their caregiver by joining the fight against Alzheimer’s. You can volunteer at your local Alzheimer’s Association office, participate in fundraising events such as the Walk to End Alzheimer’s and The Longest Day, advocate for more research funding, or sign up to participate in a clinical study as a healthy volunteer through the Alzheimer’s Association’s Trial Match. Joining the cause can help families facing the disease know that they are not alone in their fight.
Join the Fight: Honor a person living with the disease and their caregiver by joining the fight against Alzheimer’s. You can volunteer at your local Alzheimer’s Association office, participate in fundraising events such as the Walk to End Alzheimer’s and The Longest Day, advocate for more research funding, or sign up to participate in a clinical study as a healthy volunteer through the Alzheimer’s Association’s Trial Match. Joining the cause can help families facing the disease know that they are not alone in their fight.
About the Alzheimer’s Association
The Alzheimer’s Association is the world’s leading voluntary health organization in Alzheimer’s care, support and research. Our mission is to eliminate Alzheimer’s disease through the advancement of research; to provide and enhance care and support for all affected; and to reduce the risk of dementia through the promotion of brain health. Our vision is a world without Alzheimer’s. For more information, call our 24/7 Helpline at 800.272.3900 or visit alz.org.
In Michigan, Lyme disease is the most commonly reported tick-borne disease. It is spread by an infected blacklegged (deer) tick. Most humans are infected through the bites of immature ticks called nymphs that feed during the spring and summer months. Nymphs can be difficult to see since they are approximately the size of a poppy seed. In most cases, the tick must be attached for 36 to 48 hours or more before the Lyme disease bacterium can be transmitted. “Prompt removal of ticks is the best method to decrease the chance of Lyme disease,” said Dr. Paul Heidel, the medical director of the Ottawa County Department of Public Health. “Seek medical attention if you develop a fever, a rash, severe fatigue, facial paralysis, or joint pain within 30 days of being bitten by a tick.”
The most important way to protect against Lyme disease is to prevent tick bites.
Avoid direct contact with ticks
• Walk in the center of trails.
• Avoid wooded and brushy areas with high grass and leaf litter.
• Create tick-safe zones in your yard. Keep patios and play areas away from vegetation, regularly remove leaves, clear tall grasses and brush around home, place wood chips or gravel between lawns and wooded areas, and use a chemical control agent.
Use insect repellent
• Apply repellent containing DEET (20-30 percent) or Picaridin on exposed skin.
• Treat clothing and gear (such as boots, pants, socks and tents) with products containing 0.5% permethrin. Do not use permethrin directly on skin.
• Always follow the manufacturer’s instructions when applying any repellents.
Find and remove ticks
• Bathe or shower after being outside in tick-infested areas (preferably within two hours).
• Conduct a full-body tick check (under arms, in and around ears, inside belly button, behind knees, between legs, around waist and especially in hair).
• Examine gear and pets. Ticks can ride into the home on clothing and pets, and then attach to a person later. Use tick prevention products on your pets.
• Wash clothing in hot water and dry on high heat after being outside to kill ticks.
• Use fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible. Pull upward with steady, even pressure. Don’t twist or jerk the tick; this can cause the mouth parts to break off and remain in the skin. Clean the area with rubbing alcohol, an iodine scrub or soap and water.

“Tick checks are recommended after any hike, but especially one along the lake shore,” said John Scholtz, the director of Ottawa County Parks & Recreation.
For more tick and Lyme disease information, please visit www.cdc.gov/lyme or www.michigan.gov/lyme.
Guide – Ticks and your health: Preventing tick-borne illness in Michigan
Fact sheet – How to prevent tick bites when hiking and camping
• MDHHS_tick_guide.pdf
• CDC_Lyme-disease_HikersCampers_FACTSheet.pdf
Michael Ilgert appeals his case to the Health Services and Review Board
from EINPresswire.com.
OTTAWA, ONTARIO, CANADA, February 27, 2017 – Ottawa-area farmer Michael Ilgert is the current target of government action to curb raw milk sales. In December of 2016, Renfrew County and District Health Unit ordered Ilgert to “cease and desist from selling, offering for sale and distributing, milk that is not pasteurized.” Ilgert is now entering an appeal of the order to the Health Services Appeal and Review Board. A hearing is scheduled for Tuesday, February 28, 2017 at 10 am in the Indigo Room at the Metcalfe Hotel, 123 Metcalf Street, Ottawa, Ontario, K1P 5L9.
Ilgert is asking supporters or raw milk and food choice to show up at the hearing, call or write letters to defend consumer choice and access to farm fresh milk. See Ilgert Hit with Cease and Desist Order.
“With consumers looking for fresh, local farm foods, it is up to all of us to come out and speak up on behalf of farmers. This is especially important when our food sources are threatened and our farmers challenged,” says Elisa Vander Hout, president of Our Farms Our Food Coop, another Ontario farm which has undergone serious legal challenges for many years.
“This is the first step in what could be a long struggle for the survival of my farm. Many families depend on the food we produce,” says Ilgert.
Michael Schmidt, of Our Farms Our Food Coop, is well known for his struggle to provide raw milk to his food coop. Over the past 20 years he sacrificed valuable acreage to fund his legal costs and endured raids, seizures, and lost precious time on his farm to attend multiple court trials and hearings.
Ilgert hopes a favorable verdict on his appeal will help him avoid the same fate. “People need access to the foods of their choice from the producer of their choice. Even if those foods include farm fresh milk. I won’t back down. My job is to nourish people,” declares Ilgert.
Our Farms, Our Foods Coop is a 200 member cooperative formed for the purpose of boarding personal cows with a responsible dairyman. The group is just one of the many interested stakeholders in changing Canadian policy on raw milk. For additional information on raw milk realmilk.com For more on this case see The Bovine blog.
For those who have a loved one with Alzheimer’s or dementia, the thought of holiday get-togethers with family and friends may leave you feeling exhausted, anxious, or just plain overwhelmed. And while it can be a challenging time of year, with some planning and adjusted expectations, your celebrations can still be happy, memorable occasions.
According to data just released in the 2015 Behavioral Risk Factor Surveillance System, in Michigan, one in eight of those aged 45 and over report they are experiencing confusion or memory loss that is happening more often or is getting worse. For those with worsening memory problems, 45.5 percent say it created functional difficulties, such as causing them to give up day-to-day, work or social activities. With Alzheimer’s disease becoming more common, it is more likely that someone with Alzheimer’s disease will be in attendance at your holiday gathering and it is important to be prepared.
Here are our top tips for surviving the holiday season with loved ones with Alzheimer’s or dementia:
1. Let guests know what to expect before they arrive. Sending a letter or email in advance, letting people know about what to expect and how they can help will ease some of the burden when guests arrive. In the early stages of Alzheimer’s, family can help with communication by being patient, not interrupting or correcting, and giving the person time to finish his or her thoughts. In the middle or late stages, make sure visitors understand that changes in behavior and memory are caused by the disease and not the person. For ideas on how to let others know about changes in your loved one, join ALZConnected, our online support community, where caregivers share tips on what has worked for them.
2. Pare down your responsibilities. The stress of caregiving layered with holiday traditions can take a toll. Give yourself permission to do only what you can reasonably manage. If you’ve always invited 15 to 20 people to your home, consider paring it down to a few guests for a simple meal. Let others contribute. Have a potluck dinner or ask them to host at their home. You also may want to consider breaking large gatherings up into smaller visits of two or three people at a time to keep the person with Alzheimer’s and yourself from getting overtired. Make sure everyone understands your situation and has realistic expectations about what you can do.
3. Avoid triggers. If evening confusion and agitation are a problem, consider changing a holiday dinner into a holiday lunch. If you do keep the celebration at night, keep the room well-lit. Make sure that you’re careful with decoration choices — blinking lights may confuse or scare a person with dementia, and decorations that look like food could be mistaken as edible. Sticking to the person’s normal routine will also help keep the holidays from becoming disruptive or confusing. Plan time for breaks and rest.
4. Keep the person involved. Focus on activities that are meaningful to the person with dementia. They may find comfort in singing old holiday songs or looking through old photo albums. As the person’s abilities allow, invite them to help you prepare food, wrap packages, help decorate or set the table. This could be as simple as having the person measure an ingredient or hand decorations to you as you put them up.
5. Look for helpful gifts. Diminishing capacity may make some gifts unusable or even dangerous to a person with dementia. If someone asks for gift ideas, suggest items the person with dementia needs or can easily enjoy. Ideas include: an identification bracelet, comfortable clothing, their favorite music, videos and photo albums.
6. Bring the celebration to a care facility. A holiday is still a holiday whether it is celebrated at home or at a care facility. If your loved one isn’t able to celebrate at home, consider joining your loved one in any facility-planned holiday activities. Bring a favorite holiday food to share. Sing holiday songs and ask if other residents can join in, or read a favorite holiday story or poem out loud.
To learn more ways to make the holidays peaceful and joyous with a loved one with dementia, visit www.alz.org, or call our 24/7 helpline at 800.272.3900.
About the Alzheimer’s Association
The Alzheimer’s Association is the world’s leading voluntary health organization in Alzheimer’s research, care and support. Our mission is to eliminate Alzheimer’s disease through advancement of research, to provide and enhance care and support for all affected, and to reduce the risk of dementia through the promotion of brain health.
Harbor Hospice Makes More Meaningful Moments Possible
(West Michigan) – November is National Hospice and Palliative Care Month and hospices across the country are reaching out to raise awareness about the highest quality care for people coping with life-limiting illness.
“Every year, nearly 1.6 million people living with a life-limiting illness receive care from hospice and palliative care providers in this country,” said J. Donald Schumacher, president and CEO of the National Hospice and Palliative Care Organization. “These highly-trained professionals ensure that patients and families find dignity, respect, and love during life’s most difficult journey.”
Hospice is not a place. Hospice and palliative care programs provide pain management, symptom control, psychosocial support, and spiritual care to patients and their families when a cure is not possible. These programs combine the highest level of quality medical care with the emotional and spiritual support that families need most when facing the end of life. Through this specialized quality care, we see many patients and their families experience more meaningful moments together. Hospice helps them focus on living despite their diagnoses.
“Hospice and palliative care is not about taking care of a disease it is about taking care of people. Our nurses, nurse’s aides, physicians, social workers, spiritual care and volunteers support and care for the patient and family during this difficult time.” Kelly St. Martin LMSW, Clinical Outreach Specialist for Harbor Hospice.
As Kathy Huffman, a Harbor Hospice volunteer noted, “I’m very grateful to be part of this organization. Every time I go on a patient visit to give, I always walk away having received!”
“Many of our volunteers have experienced the benefits of hospice care firsthand. I love to hear their stories of how we helped care for their loved ones. Because of that quality of care, they now want to become a Harbor Hospice volunteer to help provide that same kind of care for our patients” Paula Poel, Harbor Hospice Volunteer Coordinator.
More information about Harbor Hospice, palliative care, advance care planning and volunteering is available by calling 231.728.3442 or 800.497.9559.
Stories showing the many ways hospice makes more special moments possible can be found at www.momentsoflife.org. See more Harbor Hospice moments at facebook.com/HarborHospice or www.HarborHospiceMI.org
Teens consistently say parents—not peers, not partners, not popular culture
most influence their decisions about relationships and sex.
1. Be open
2. Be the expert
3. Be accessible
4. Be trusting
5. Stay calm
6. Ask open-ended questions
7. Listen to your teen
8. Put yourself in their shoes
9. Appeal to common goals
10. Show your interest
New report highlights health gaps among state countiesDetails strategies for improvement – www.countyhealthrankings.org
Ottawa County—There are substantial health differences among Michigan counties, and eliminating those differences could prevent more than 7,800 premature deaths every year, according to a State Health Gaps report released today by the Robert Wood Johnson Foundation (RWJF) and the University of Wisconsin Population Health Institute (UWPHI).
The report also looked at a total of 30 important factors that contribute to how long and how well people live, and found that in Michigan opportunities for health vary widely from county to county. In 2015, Ottawa County ranked 1st out of 82 counties in Michigan for healthy people, according to the sixth annual County Health Rankings http://bit.ly/1xihJqj
If every county in Michigan did as well as the counties in the state
that performed best on these important health factors, there could be:
• 287,000 fewer adult smokers
• 294,000 fewer adults who are obese
• 259,000 fewer adults who drink excessively
• 167,000 fewer people who are uninsured
• 180,000 more adults, ages 25-44, with some education beyond high school
• 79,000 fewer people who are unemployed
• 186,000 fewer children in poverty
• 34,000 fewer violent crimes
• 181,000 fewer households with severe housing problems
The Health Gaps report is one of 50 released today. Each identifies significant gaps in opportunities for good health among counties within every state. Each state report details how well the healthiest counties do; the difference that could be made if every county had the same chance to be healthy; and strategies to close the gaps between the healthiest and least healthy places. The full report for the state of Michigan can be found at www.countyhealthrankings.org./health-gaps.
The Michigan Health Gaps Report is a product of the County Health Rankings & Roadmaps program. The program offers data, tools, and resources to help communities throughout their journey to build a Culture of Health.
10 Tips for Parents:

Be open.
Be the expert.
Be accessible.
Be trusting.
Stay calm.
Ask open-ended questions.
Listen to your teen.
Put yourself in their shoes.
Appeal to common goals.
Show your interest.
The national public education campaign is celebrated in October and coordinated by Advocates for Youth. Ottawa County Department of Public Health (OCDPH) encourages parents and care givers to continue talking with youth about how to make good decisions about sex, contraception and pregnancy.
Parents are the best sexuality educators for their children.
Teens consistently say that parents most influence their decisions about sex.
Parents want to be good sex educators, but may not always know how.
It is possible to be an ask able adult.

According to the 2013 Ottawa County Youth Assessment Survey, the average age of students who first had oral sex or sexual intercourse was 15 ½. By 12th grade, 47% of students had engaged in oral sex, 40% in sexual intercourse and 37% in sexting. www.miOttawa.org/2013YAS
In 2013, Ottawa County had 243 teen pregnancies, with only 68% being live births (166 babies born). Of these, 37 were repeat teen pregnancies (26 live births).
The high rate of chlamydia cases
in Ottawa County is also a health issue.
In 2014, there were 704 positive cases of chlamydia.
“We know it can be difficult to have conversations about sensitive topics,
but it is important for parents to talk with their children about abstinence
and sexuality.” Heather Alberda, OCDPH
Sexuality Educator www.miOttawa.org/SexEd
For more information, please contact Heather Alberda, Sexuality Educator
at halberda@miottawa.org or 616-393-5774.
Keep talking! @advocates4youth Parent & youth sexual health talks http://bit.ly/1wJ1sHJ www.miOttawa.org/SexEd @miOCDPH
Sources
OCDPH Parent’s Guide to Engaging in a Sexual Health Conversation http://www.miottawa.org/Health/OCHD/pdf/FamilyGuide.pdf
Let’s Talk Resources
http://thenationalcampaign.org/event/let%E2%80%99s-talk-month
Ottawa County – Michigan’s Public Health Code requires children 3 – 5 years of age to have a hearing and vision screening prior to kindergarten entry. The Ottawa County Department of Public Health’s (OCDPH) Hearing & Vision program focuses on the importance of early detection and offers free screening services to school aged children. Comprehensive screenings are conducted by fully trained hearing and vision technicians. Last year, OCDPH referred 8% of all children vision screened and nearly 3% hearing screened to a specialist. Parents registering their child in kindergarten or first grade must supply their school with a testing certificate. Failing to do so, will result in exclusion from school. www.miottawa.org/hearingvision
1. Hearing and vision loss can impede a child’s development and performance.
2. Early detection may lead to better care and treatment.
3. Hearing and vision are vital to learning, working and socialization.
4. Proper hearing and vision enables children to reach their full potential.
5. Every dollar invested in screenings saves Michigan $112 in hearing and $162 in vision costs. (Values are based on health care costs and future productivity loss.)
“After your vision referral to an eye doctor, our daughter received her first pair of glasses. Thank you so much for letting us know about her difficulties, as it was not something she had previously expressed. We appreciate it!”
– OCDPH Hearing & Vision client
Suggested Tweet:
Hearing & vision loss can hinder child development. Call 616-396-5266
for appt.- mandatory for Pre-K & K @miOCDPH miOttawa.org/hearingvision
Hackley Community Care is excited to offer Centering Pregnancy at their health center. Centering Pregnancy is a model of care developed by the Centering Healthcare Institute that integrates three components of prenatal care within a group setting: health assessment, education and support.
The model brings together women that are in the same trimester of their pregnancy in a group setting where they will learn care skills for themselves and their infants during their pregnancy, their births and the postpartum period. All Centering Pregnancy groups are facilitated by an OB provider. The group consists of 8-12 pregnant women expected to deliver around the same time, and they have the opportunity to develop a support network with other group members.
Centering is unique in that the expectant mother receives her assessments through self-care activities within the group with other moms. The group also has the opportunity to discuss and problem-solve topics and concerns related to their pregnancy, nutrition, and the opportunity to motivate and empower each other. This creates a safe, trusting environment that establishes sustained relationships and support. Centering Pregnancy sessions are ten weeks in duration and each session lasts about two hours. Expectant mothers can also bring their support person if they like. After delivery, new mothers also receive post-partum care counseling and breastfeeding support if they choose to do so.
Implementing the Centering Pregnancy model allows Hackley Community Care to impact the health status of pregnant women by providing learning skills to ensure the expectant mom has a healthy baby. When expectant moms have healthy babies, this also improves the county overall health status of low birth weight babies, and increases breastfeeding rates.
Hackley Community Care will begin their Centering Pregnancy sessions in June of 2015 and they are currently registering expectant moms. If you are an expectant mother and interested in participating in Centering Pregnancy, please call our OB and Women’s Health Services Department at 231.737.1335 Ext. 6655 to register and obtain more information.
To learn more about Hackley Community Care, please visit our website at www.hackleycommnitycare.org . You can learn more about the Centering Healthcare Institute at www.CenteringHealthcare.org .
The California Medical Association (CMA) recently dropped their decades-long opposition to assisted suicide after a bill to legalize assisted suicide was introduced in California.
In their announcement the CMA says they are changing their position on assisted suicide to “neutral,” but the reasoning behind their statement uses the rhetoric of organization’s that promote the legalization of assisted suicide and euthanasia.
The CMA press release announcing their decision is filled with absurd attempts to gloss over their disregard for the lives of those considering suicide. Their arguments sound eerily like the rhetoric and euphemisms used to defend abortion-on-demand. Assisted suicide is called “physician aid-in-dying” or “end of life options.” The relationship between doctor and patient is exalted. Helping someone kill themselves is equated with methods of “treatment.”
Important issues that previously led the California Medical Association to oppose assisted suicide are not mentioned or refuted. Those issues include the potentials for abuse, the recognition that desire for suicide is not a rational decision, fears that legalizing assisted suicide could undermine hospice care, the uncertainly of medical diagnoses, and how assisted suicide violates the fundamental “do no harm” medical ethos.
On June 4, the California Senate voted in favor of a bill that would legalize assisted suicide in California for terminally-ill patients. If it passes the California State Assembly and is signed by Governor Jerry Brown, California would join the small group of states where assisted suicide is legal: Oregon, Washington and Vermont. In Montana, a judicial ruling prevents doctors from being prosecuted under state law if they help a patient kill themselves.
In 2012, 85 individuals in Oregon used lethal doses of prescription drugs to legally kill themselves. This number has risen nearly every year. The population of Oregon is roughly a tenth of California, meaning if California approves the assisted suicide law and individuals in California seek to kill themselves at the same rate as individuals in Oregon, then nearly 1000 assisted suicides a year could take place in California.
While the California Medical Association is the first state medical association group to announce they are “neutral” on physicians helping to kill patients, only time will time if they are the last as our society grows in its comfort with embracing suicide as an acceptable way to treat the weak and vulnerable.
Learn more about the dangers of assisted suicide and euthanasia at www.rtl.org.
Twitter | Facebook | Blog | YouTube
Ottawa County –According to the Michigan Department of Human Services, a baby dies every three days in Michigan and these deaths are 100% preventable. Sudden Infant Death Syndrome (SIDS) is the leading cause of deaths for babies less than one year of age. Rick Snyder, governor of Michigan, proclaimed September as Infant Safe Sleep Awareness Month in Michigan.
The Michigan Department of Community Health, Education and Human Services and local agencies, such as the Ottawa County Department of Public Health Maternal & Infant Health & Prenatal Education (MIHP) program and Pathways, MI are working together to raise awareness and educate parents about safe sleep practices. “Infants do not have enough strength to pull themselves out of places where they might get wedged,” said Leigh Moerdyke, Community Youth Development Program Director at Pathways, MI. She said when babies are placed on their stomachs to sleep it tips their chin and neck, closing off the airway and potentially causing asphyxiation.
Safe Babies
1. Always place your baby on his or her back for naps and at night.
2. Babies should not sleep in an adult bed, on a couch or in a chair with anyone.
3. Use a firm mattress in a safety-approved crib with a fitted sheet.
4. Keep soft objects, toys, crib bumpers and loose bedding out of sleeping environments.
5. Babies need tummy time when he or she is awake with someone watching.
Healthy Babies
1. Women should receive regular healthcare during their pregnancy.
2. Do not smoke, drink alcohol or use drugs during pregnancy or after your baby is born.
3. Breast-feed your baby to reduce the risk of SIDS.
4. Do not let your baby get too warm during sleep.
5. Follow your doctor’s recommendations on child immunizations.
Dawn Dotson, Community Health Supervisor
Maternal & Infant Health & Prenatal Education
Ottawa County Department of Public Health
616-393-5737 ddotson@miottawa.org
(Condensed from an article in the February, 2014 Reader’s Digest Magazine by Dr. Joel K. Kahn, author of the Holistic Heart Book)
• Have five cups of fruit and vegetables per day.
• Drink three cups of green, black or oolong tea a day
• Don’t eat processed meat
• Don’t eat much meat
• Eat sardines, mackeral, anchovies, salmon and herring
• Love a pet
• Sit in a sauna (preferably infrared)
• List something you are grateful for every day and read the list once a week
• Men: Have sex twice a week
• Open windows to air our your house regularly
• Clean your kitchen with items you would cook with (i.e. white vinegar, baking soda, lemon, cornstarch)
• Cook and store food in glass, ceramic or stainless steel.
Read the whole article here: http://www.rd.com/slideshows/how-to-prevent-heart-disease/
Two cases of E. coli 0157:H7 in West Michigan have been traced back to consumption of raw milk products from an Ottawa County cow share program. In March, a 31 year old Muskegon County woman became ill after drinking raw milk, and in April, a 6 year old child from Kent County became ill after possible consumption of the raw milk product.
Organisms that make people sick are found in the intestines of animals. Contamination of milk occurs when fecal matter is present on the udder of an animal or in the equipment used to process the milk. Enough bacteria to cause illness can be present and not be visibly dirty upon inspection. Pasteurizing is the process of heating the milk to high temperatures to kill the harmful bacteria that make you sick. Raw or unpasteurized milk (sometimes called fresh milk or fresh unprocessed milk) is milk that comes directly from a cow, goat, sheep or other animal’s udder and is not heat treated (pasteurized) to kill bacteria. Raw milk carries a much higher risk of causing serious illness than pasteurized milk, and you cannot see or smell the germs in raw milk that make you sick.
Some believe drinking raw milk products is more nutritious and provides the body with “good bacteria”. The pasteurizing process does not significantly change the nutritional value of milk, and due to the risk of serious illness, there are far safer sources of good bacteria than raw milk. Pasteurized probiotic yogurts, kefir, and other products are a great source of probiotics.
The CDC reports that unpasteurized milk is 150 times more likely to cause foodborne illness, and results in 13 times more hospitalizations than illnesses involving pasteurized dairy products. Due to poorly developed immune systems, infants and children are at greater risk for becoming sick and are more likely to suffer from long term damage from diseases linked to drinking raw milk.
Due to the health risk of consuming raw milk, it is not legal to sell raw milk or raw milk products in the State of Michigan. Because of this, raw milk is obtained through herd share programs. In a herd share program, consumers purchase a share of a cow and, as the owner of the cow, are provided raw milk from the farmer. These herd share dairy programs are not licensed or inspected by state or local agencies.
If you or someone you know has become ill in the days following consumption of a raw milk product, seek medical attention. Symptoms of illness include vomiting, diarrhea, and abdominal pain along with fever, headache, and body ache. Pregnant women, infants, small children, the elderly, and people with chronic illnesses should never consume raw milk products.
For more information on the pasteurization process:
http://www.fda.gov/Food/ResourcesForYou/consumers/ucm079516.htm
http://www.cdc.gov/features/rawmilk/
http://www.foodsafetynews.com/2014/05/raw-milk-is-ongoing-hazard-cdc-warns-public-health-workers/#.U3N_bXabXm4
By Dr. E. Kirsten Peters
Years ago I was a light smoker. Back in the day I thought nicotine did good things for my ability to think and learn. I was a serious student at the time, studying intensively seven days a week, so a powerful complement to black coffee was welcome in my life.
I both sympathize and empathize with smokers around me today. But I’m awfully glad I quit long ago, and I know many other former smokers who feel the same way. Quitting is worth all the short-term distress it can entail.
Some recent scientific news got me thinking again about smoking and how it affects both smokers and those around them. In short, there’s plenty of evidence that passive or second-hand smoke is detrimental to people living with smokers. That means that quitting helps not just smokers, but those who share homes (and cars) with them.
Recently the European Heart Journal published a study about the effects of parental smoking on kids. The research focused on some 2400 children in a cohort in Finland and over 1300 in a group in Australia. Researchers noted the smoking behavior of parents — whether the adults were non-smokers, or if one or both of them smoked. When the kids grew up, the researchers examined the kids’ arteries via ultrasound exams.
The study found that artery walls were thicker in kids who had grown up in homes where both parents smoked. Thicker arteries are bad news, making for greater risk of strokes or heart attacks. On average, the kids who grew up in homes where both parents smoked had arteries that were 3.3 years “older” than those who grew up in smoke-free homes. These changes were permanent — a sobering fact to contemplate for any parent (and I might add, any grandparent around the grandkids).
Dr. Seana Gall, lead author of the study, told ScienceDaily, “Parents…should quit smoking. This will not only restore their own health but also protect the health of their children into the future.”
There was further bad news for kids who had two parents who smoked.
“Those with both parents smoking were more likely, as adults, to be smokers or overweight than those whose parents didn’t smoke,” Gall said.
Once again, the news from the world of medical research suggests it’s time for people to quit smoking. If you smoke and you have kids (or grandkids) to consider, please talk with your health care provider about an approach to help you kick the habit. Even if you’ve tried in the past to quit but have failed, this next effort could set you free. It took me more than one attempt to quit, but it was one of the best things I did back in the day.
I know first-hand it ain’t easy to stop smoking. But the life you save might be your own — and you could also be helping the next generation avoid permanent and harmful changes to their young bodies.
I’m pulling for both you and your family.
Dr. E. Kirsten Peters, a native of the rural Northwest, was trained as a geologist at Princeton and Harvard. This column is a service of the College of Agricultural, Human, and Natural Resource Sciences at Washington State University.